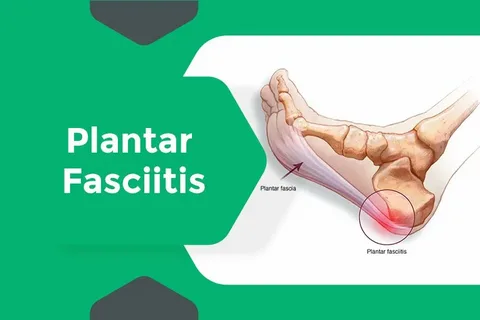
A person dealing with ongoing foot pain often seeks relief that doesn’t involve surgery. Non-surgical treatments for plantar fasciitis aim to restore comfort through gradual, targeted therapies rather than invasive methods. Each stage of the process brings distinct sensations and signs of improvement, allowing patients to understand how the healing unfolds over time.
Mild Soreness Follows Early Treatment Sessions As Tissues Adjust
At the beginning of non-surgical care, patients commonly notice mild soreness in the heel and arch areas. This is a normal response as tissues begin to adapt to therapies such as stretching, ultrasound, or shockwave treatment. A plantar fasciitis specialist explains that these reactions indicate blood flow returning to the area and the fascia fibers starting to loosen. The temporary discomfort often fades within a few days after the first sessions.
As the soft tissues adjust, the body begins rebuilding strength around the inflamed ligament. Treatments from a plantar fasciitis doctor may include light physical therapy or custom orthotics that reduce stress on the plantar fascia. This early period sets the foundation for long-term recovery by preparing the foot for improved flexibility and better load distribution.
Noticeable Relief Begins Once Inflammation Subsides Gradually
Inflammation is the primary source of pain in plantar fasciitis, and its reduction marks the first major sign of healing. Non-surgical therapies encourage natural anti-inflammatory responses through controlled stimulation of the affected area. Regular sessions with a plantar fasciitis doctor help patients feel less pressure under the heel and fewer stabbing pains during daily activity. Once swelling decreases, movement feels smoother and more natural. A plantar fasciitis specialist often adjusts treatment frequency based on the body’s progress, ensuring inflammation continues to subside without overstressing the tissue. This stage brings steady comfort, motivating patients to stay consistent with their care plan.
Gentle Mobility Returns As Fascia Tension Starts to Release
Tension in the plantar fascia can restrict movement and cause stiffness, particularly after rest. As the fascia loosens through therapy and stretching, patients regain the ability to flex and point their toes more easily. Non-surgical treatments gradually retrain the ligament to stretch without tearing, allowing greater motion and reducing morning pain.
At this point, balance and coordination exercises may be introduced. A plantar fasciitis specialist uses these routines to restore natural foot alignment, helping prevent recurrence. Increased mobility also makes it easier to return to walking, standing, or light exercise with reduced fatigue.
Patients Feel less Stiffness During Morning Steps Each Week
Morning stiffness tends to be the most persistent symptom for those with plantar fasciitis. As therapy progresses, patients often report that their first steps of the day become noticeably more comfortable. Treatments such as night splints, massage, and cold therapy improve circulation and tissue flexibility overnight.
The reduction in stiffness reflects improved elasticity of the plantar fascia. Continued sessions with a plantar fasciitis doctor reinforce these gains, ensuring the ligament remains pliable throughout the day. This improvement becomes a clear indicator that the condition is transitioning into lasting recovery.
Consistent Sessions Build Confidence in Pain-free Movement
Consistency is key in non-surgical plantar fasciitis recovery. Regular visits to a plantar fasciitis specialist allow for adjustments in therapy intensity and technique based on patient feedback. Over time, confidence replaces hesitation as pain-free walking and standing become more frequent.
As mobility improves, many patients begin incorporating light workouts or longer walking sessions. The reassurance of pain-free movement encourages long-term commitment to therapy, which helps maintain healing results. Each consistent step contributes to stronger foot mechanics and a reduced likelihood of relapse.
Supportive Footwear Brings Steadier Comfort Throughout the Day
Footwear plays a major role in sustaining recovery. Patients are advised by their plantar fasciitis doctor to wear shoes with firm arch support and cushioned soles. Proper footwear alignment minimizes tension on the fascia during long hours of activity, allowing healing to continue even outside treatment sessions.
Many individuals notice that switching to supportive shoes eliminates mid-day soreness and helps them remain active longer. The right pair complements therapy efforts, keeping the fascia stable and reducing irritation from impact. Over time, footwear support becomes an integral part of maintaining comfort.
Treatment Intervals Shorten As Healing Becomes More Stable
As improvement solidifies, treatment sessions are spaced farther apart. The plantar fasciitis specialist evaluates progress and may shift from weekly therapy to biweekly or monthly maintenance. This transition marks the body’s growing ability to sustain recovery independently.
Shorter intervals do not mean less care; rather, they signal that tissues are healing efficiently. A plantar fasciitis doctor continues monitoring flexibility, inflammation, and gait to ensure progress holds steady. Patients often find this stage empowering, as it confirms that their body’s natural healing mechanisms have strengthened.
Sensitivity Around the Heel Decreases with Regular Therapy
One of the most satisfying milestones for patients is the reduction of heel sensitivity. Gentle pressure that once triggered sharp pain now feels tolerable, indicating that nerve irritation is subsiding. Treatments focusing on circulation and tissue repair help desensitize the heel over time.
The disappearance of tenderness allows normal movement without hesitation. Continued visits to a plantar fasciitis specialist help preserve these improvements, ensuring that the fascia remains healthy and resilient. Regular therapy supports complete restoration of function and provides lasting relief from discomfort.